A basal-bolus insulin regime is used to mimic the body’s normal insulin production as closely as possible. It should allow you more flexibility, and eat what and when you want to, and even miss a meal if you don’t want to eat, while still keeping good control of your blood sugar level.
Other people and some healthcare professionals may refer to blood sugar as blood glucose.
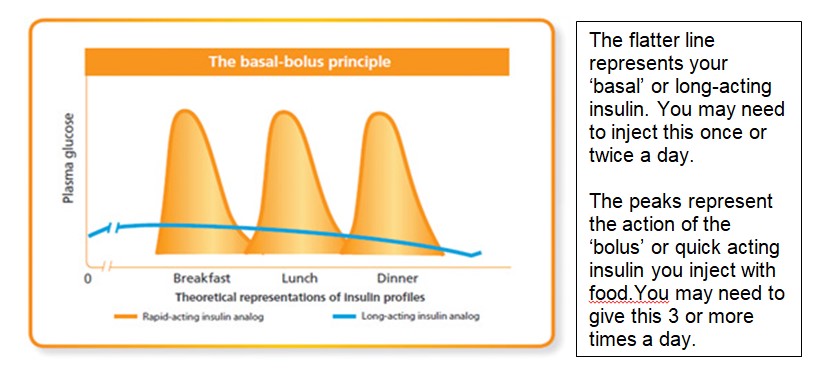
Insulin actions
What is basal insulin?
Your body needs a basic amount of insulin all the time – day and night – even between meals. This is called ‘basal’ insulin. It controls your blood sugar at times when you are not eating but when your body still needs energy. Basal insulin is usually injected once per day at bed-time, but may need to be injected twice a day, as it may not last for 24 hours in some people.
Types of basal (long acting) insulin
- Intermediate acting (Isophane) insulin e.g. Insulatard, Insuman Basal Humulin I and Hypurin Porcine Isophane
These insulins look cloudy and need to be mixed well before use. They begin to work about 2 hours after injection, peak between 4-6 hours and last for approximately 8-14 hours. They are usually injected twice a day.
- Long-acting analogue insulin e.g. Lantus, Levemir or Abasaglar
These insulins are clear in appearance and don’t need mixing or shaking before injection. They are longer lasting than intermediate-acting (isophane) insulins and begin to work about 2 hours after injection, have little or no peak action, and last for approximately 18-24 hours. These insulins are injected once or twice a day.
- Ultra long-acting analogue insulin g. Tresiba and Toujeo
Like long-acting insulin analogues, these are clear in appearance. They last for longer than long-acting analogue insulins: Toujeo lasts for up to 27 hours and Tresiba for up to 42 hours. They are injected once a day, and can be taken at any time of the day, but preferably at the same time each day. They don’t need to be taken with food because they don’t have a peak action. These insulins come in different strengths of insulin, so it is important to check that the right strength of ultra long-acting analogue insulin has been prescribed for you by your doctor or diabetes specialist nurse.
What is bolus (quick acting) insulin?
Bolus insulin is usually injected just before you eat a meal. When you eat a meal containing carbohydrate food (e.g. bread, potato, cereals, fruit, etc.) your blood glucose level rises as the carbohydrate food is turned into glucose. Insulin is like a key and unlocks the cell doors to move glucose move from the blood stream into the body’s cells to make energy. You need ‘bolus’ insulin to cope with the rise in your blood glucose level after eating.
Types of bolus insulin
- Ultra fast acting insulin e,g, Fiasp
- Rapid acting analogue insulins e.g. Novorapid , Humalog or Apidra
- Short acting insulins – e.g. Insuman Rapid or Humulin S
Different types of bolus insulins have different actions. Your diabetes health care professional will advise you when to inject them in relation to when you eat your meals as some need to be injected up to 15-30 minutes before you eat.
How much bolus insulin should I give?
Some people may be on set doses of bolus insulin at mealtimes. Others may adjust their insulin doses depending on what they have to eat, their blood sugar levels and how active they plan to be. Your diabetes specialist nurse / dietician will discuss with you what is the best option for you
General principles for the adjustment of insulin
- Observe the pattern in your blood sugar levels – it is useful to check your blood sugar levels on waking, before each meal and at bedtime for at least 2-3 days before adjusting your insulin doses.
- Ideally your blood sugar levels should be between 4-7mmols/l before meals and 6.5 – 8 mmols/l before bed. Your individual blood glucose targets should be discussed with you by your diabetes healthcare professional.
- During illness and stress you may find your blood sugar level rises and you may need to increase your insulin doses
- Insulin can be adjusted in advance if you anticipate changes in your physical activity. You may find that you need to adjust your insulin doses before, during and for several hours after exercise – your doctor, diabetes specialist nurse or dietitian will be able to advise you if this is necessary.
Why are blood sugar levels sometimes high?
A temporary high blood sugar level from time to time is impossible to avoid in everyday life.
Reasons for high blood sugar levels include:
- Illness / infection
- eating more carbohydrate than usual at a meal or for a snack
- stress
- steroid therapy
- missed insulin / not enough for the food eaten
- problem with injection technique or sites being lumpy
- Less active than usual
- Snacking between meals
General guidelines about insulin adjustment for high blood sugars
Observe patterns in blood sugar levels for 2-3 days. If the pattern of blood sugar level is above 7mmol/L before mealtime increase the insulin dose e.g. if blood sugar level pattern is:
- high at lunchtime increase the breakfast insulin dose
- high at teatime increase the lunchtime insulin dose
- high at bedtime increase the evening meal insulin dose
- high at breakfast time usually indicates increasing the basal insulin dose if you are sure you’re not going low in the night
You may wish to discuss any changes with the Diabetes Team first
Observe patterns in blood sugar levels for 2-3 days. If the pattern of blood sugar level is above 7mmol/L before mealtime increase the insulin dose e.g. if blood sugar level pattern is:
- high at lunchtime increase the breakfast insulin dose
- high at teatime increase the lunchtime insulin dose
- high at bedtime increase the evening meal insulin dose
- high at breakfast time usually indicates increasing the basal insulin dose if you are sure you’re not going low in the night
Why are blood sugar levels sometimes low?
Reasons for low blood sugar levels include:
- not enough or no carbohydrate at a meal
- too much insulin for the amount of carbohydrate eaten
- increased or unexpected physical activity
- alcohol
- problem with injection technique or sites being lumpy
- Hot weather / baths / showers
General guidelines about insulin adjustment for low blood sugars
If you have unexplained hypoglycaemia *(low blood sugar below 4mmol/L) insulin should be reduced. If you know the reason for a low blood sugar level then take action to prevent it from happening again. Otherwise, if blood sugar level is:
- low at lunchtime reduce the breakfast insulin dose.
- low at teatime reduce the lunchtime insulin dose
- low at bedtime reduce the evening meal insulin dose
- low at breakfast time or during the night means reducing basal insulin dose
You may wish to discuss any changes with the Diabetes Team first
An decrease of 1-2 units is generally recommended, or 10 – 20 per cent if you are on large doses of insulin at mealtimes.
What to do if your blood sugar level is low (below 4mmol/L)?
Where possible do a blood test to confirm this and then follow the instructions below:
Blood test confirms your blood glucose is 4mmols/l or less
Step 1
Take immediately either
• 150 mls of normal coke or lemonade or other non-diet fizzy/still drink
or
• 200 ml Lucozade Energy
or
• 200 ml carton of fruit juice
or
• 3-4 teaspoons of sugar dissolved in warm water, tea or coffee (not milk)
or
• 3-4 jelly babies, chewy sweets or fruit pastilles
or
• 4-5 GlucoTabs or 5-6 Dextrose tablets
Retest your blood glucose after 15 minutes, if less than 4mmols/l repeat Step 1 until it rises above 4mmols/l , remembering to keep testing every 15 minutes
Step 2
Once your blood glucose level is above 4mmols/l eat your next meal if this is due or have a slower releasing carbohydrate snack such as:
• 2 plain digestive biscuits
• A slice of toast
• A banana
• a small bowl of cereal with milk
• cereal bar
Note
Recurrent ‘hypos’ or a pattern of ‘hypos’ should be discussed with your diabetes team as your insulin treatment may need changing. Any severe ‘hypos’ requiring help from another person, paramedic or medical staff must be discussed with your diabetes team the following day.
Calling us for review
It is important that you keep in touch with us on a regular basis so that we can support you with the changes to your insulin treatment. Once things are more stable you can ring us when you need.
For the south team, telephone the Salisbury office on 01722 425176
For the north team, telephone the Chippenham office on 01249 456483.
It is likely that you will need to leave us a message requesting a call back as team members may be attending clinics and seeing other patients.